The guys from HelpMeSee have developed an alternative to Eyesi for manual small incision cataract surgery. Not sure if the target developing countries will have the access to it, but it’s just the beginning…
Theatre performance
I have never thought how OP-time can be evaluated and banchmarked. Such things as under- oder overrun (ending too early or too late), utilisation and cancellation rates can be assessed and compared to the recommended standards.
Here is a good study from the South Africa:
”
Operating theatre efficiency at a tertiary eye hospital in South Africa
S Afr Med J. 2023 May 5;113(5):59-64. doi: 10.7196/SAMJ.2023.v113i5.16602.
Authors
M Tsimanyane 1 , K Koetsie 1 , A Makgotloe 1
Affiliation
1 Department of Ophthalmology, Charlotte Maxeke Johannesburg Academic Hospital and Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa. khlcyn001@gmail.com.
PMID: 37170602
DOI: 10.7196/SAMJ.2023.v113i5.16602
Abstract
Background: South Africa (SA) is a resource-limited country that needs efficient operating theatres in order for surgical care to function cost-effectively. Regular assessment of theatre efficiency in our setting is therefore needed.
Objectives: To describe ophthalmology theatre efficiency at a central hospital in SA and compare this with international benchmarks.
Methods: St John Eye Hospital is the ophthalmology section of Chris Hani Baragwanath Academic Hospital in Soweto, SA. It has three operating theatres. A cross-sectional study was done of the theatres’ registry of surgical procedures over a 6-month period. Data analysed included the starting and finishing times of theatre lists, surgical cases that were cancelled on the day of surgery, and theatre utilisation rates. These data were compared with international benchmarks.
Results: A total of 1 482 surgical procedures in 229 theatre lists were included in the study. Sixty-five percent of these theatre lists started late, accounting for 4 236 minutes of lost theatre time, significantly more than the maximum of 10% recommended by the Royal College of Anaesthetists. Of theatre lists, 23% and 30% finished after 16h15 (theatre overrun) and before 16h00 (theatre underrun), respectively. This is more than double the 10% recommended by the Royal College of Anaesthetists. The theatre utilisation rate was 62%, which is significantly lower than the ideal utilisation rate of 80%. The cancellation rate was 16%, which is significantly higher than the international benchmark of 2% recommended by the New South Wales guidelines. The most common reasons for cancellations were medical unfitness of the patient and lack of operating theatre time.
Conclusion: All theatre efficiency parameters at St John Eye Hospital were below international benchmarks”
Normal glaucoma surgical rate in Africa?
50 trabs per one million of population. So little must be done to improve glaucoma management, according to review from West African studies.
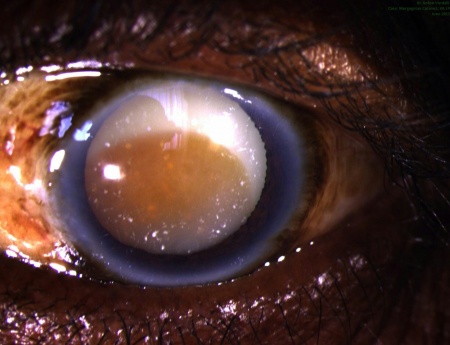
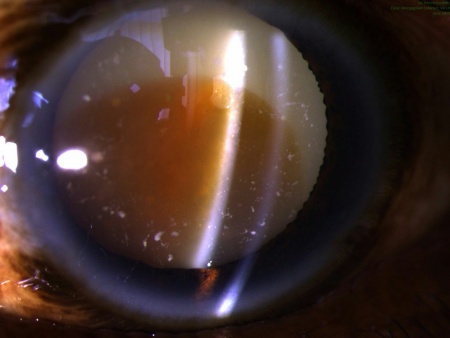
Morgagnischer Staar (morgagnian cataract)
Zuweilen soll das Trübwerden des Morgagnischen Liquor den Staar, welcher alsdann Morgagnischer Staar (Cataracta Morgagniana s. intertitialis) genannt wird, bedingen; dieses Uebel wird aber selten beobachtet, da Trübungen des Morgagnischen Dunstes schnell die Verdunklungen der Linse bedingen.
Quelle: Beck, Handbuch der Augenheilkunde (1823), S. 258-259