Steffen J1, Coupland SE2,3, Smith JR4.
Author information:
1. Division of Ophthalmology, University of Cape Town, Cape Town, South Africa.
2. Institute of Translational Medicine, University of Liverpool, Liverpool, UK.
3. Liverpool Clinical Laboratories, Liverpool University Hospital NHS Foundation Trust, Liverpool, UK.
4. Eye and Vision Health, Flinders University, Adelaide, Australia.
Abstract
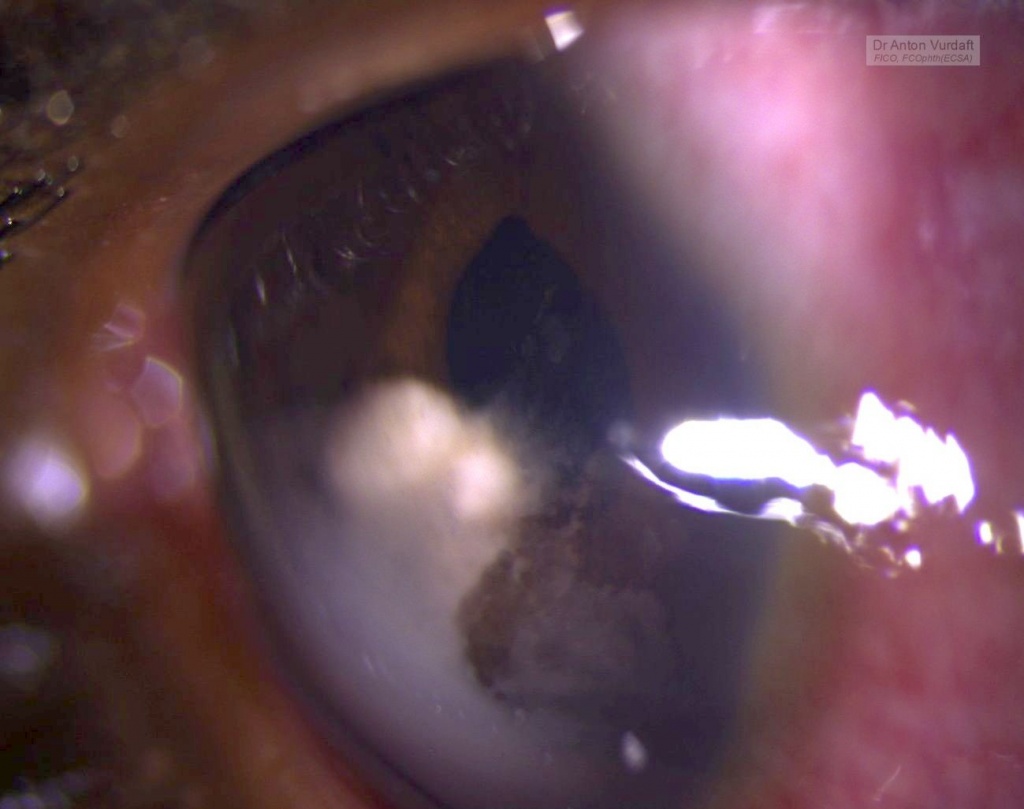
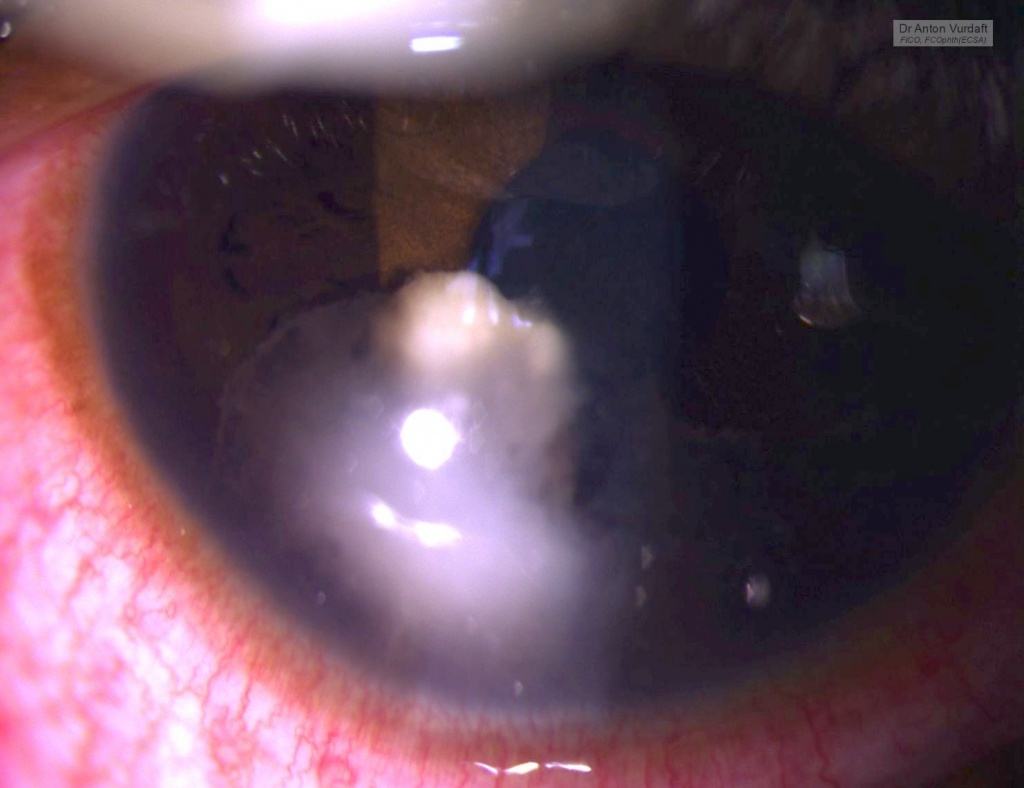
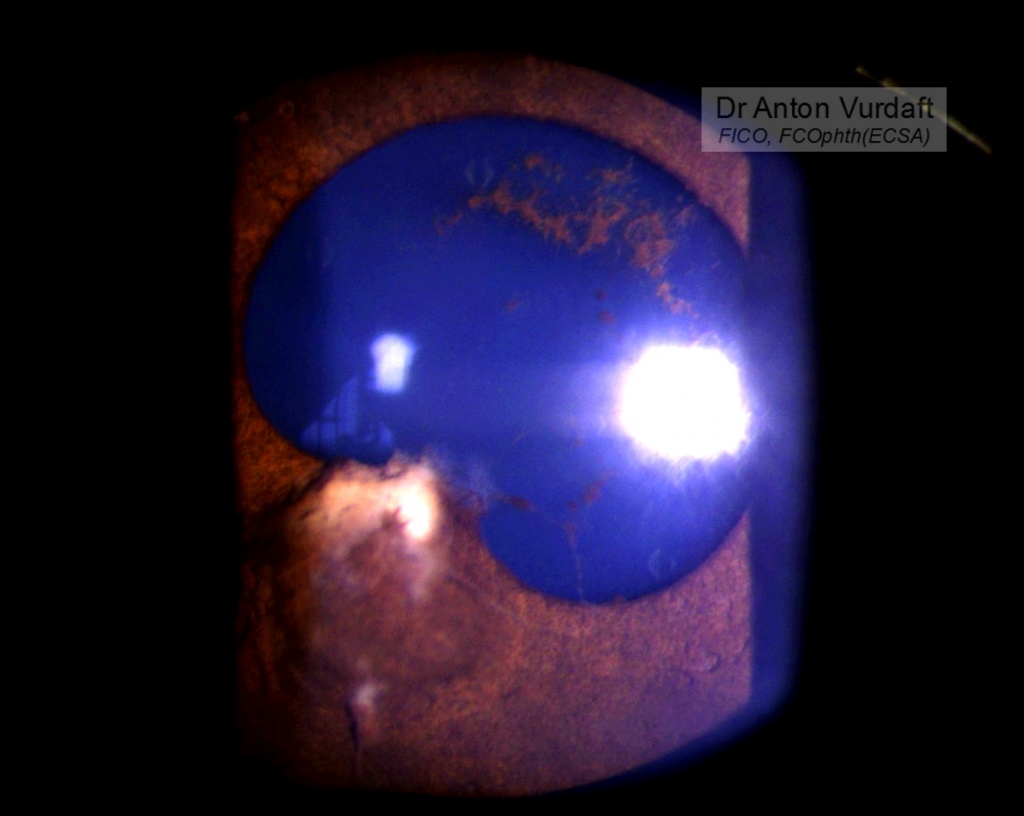
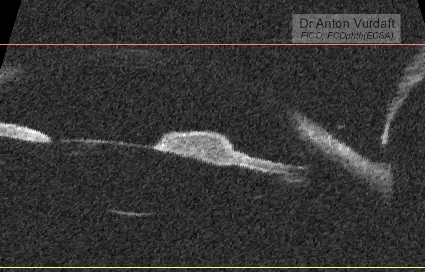
Purpose: To describe the epidemiology, clinical characteristics, diagnosis and treatment of human immunodeficiency virus (HIV)-related primary vitreoretinal lymphoma (PVRL).Methods: Narrative literature review.Results: HIV-related PVRL occurs in persons who are relatively young and generally have very low CD4+ T-cell counts. Vitritis with subretinal or sub-retinal pigment epithelial infiltrates is typical. Vitreous cytology remains the gold standard for diagnosis, supplemented by flow cytometry and genetic analyses of tumor cells, and measurement of aqueous or vitreous interleukin-10 levels. Concurrent brain involvement also may establish the diagnosis. Treatment includes antiretroviral therapy (ART), systemic chemotherapy (usually methotrexate-based) and local ocular treatment (intravitreal methotrexate, intravitreal rituximab, external beam radiotherapy). Systemic chemotherapy is of uncertain value for PVRL without other central nervous system involvement. Prognosis is poor, but has improved significantly compared to the pre-ART era. Conclusions: Ophthalmologists should consider the diagnosis of PVRL in HIV-positive individuals who present with intermediate or posterior uveitis.