![]() EN: A case of June 2016. A 10yo boy injured himself with a fish-hook during fishing. With these hooks people catch the tasty “mbufu” fish und occasionally even a tiger-fish in Zambesi river. The hook entered through sclera near limbus and left the eye through central cornea.
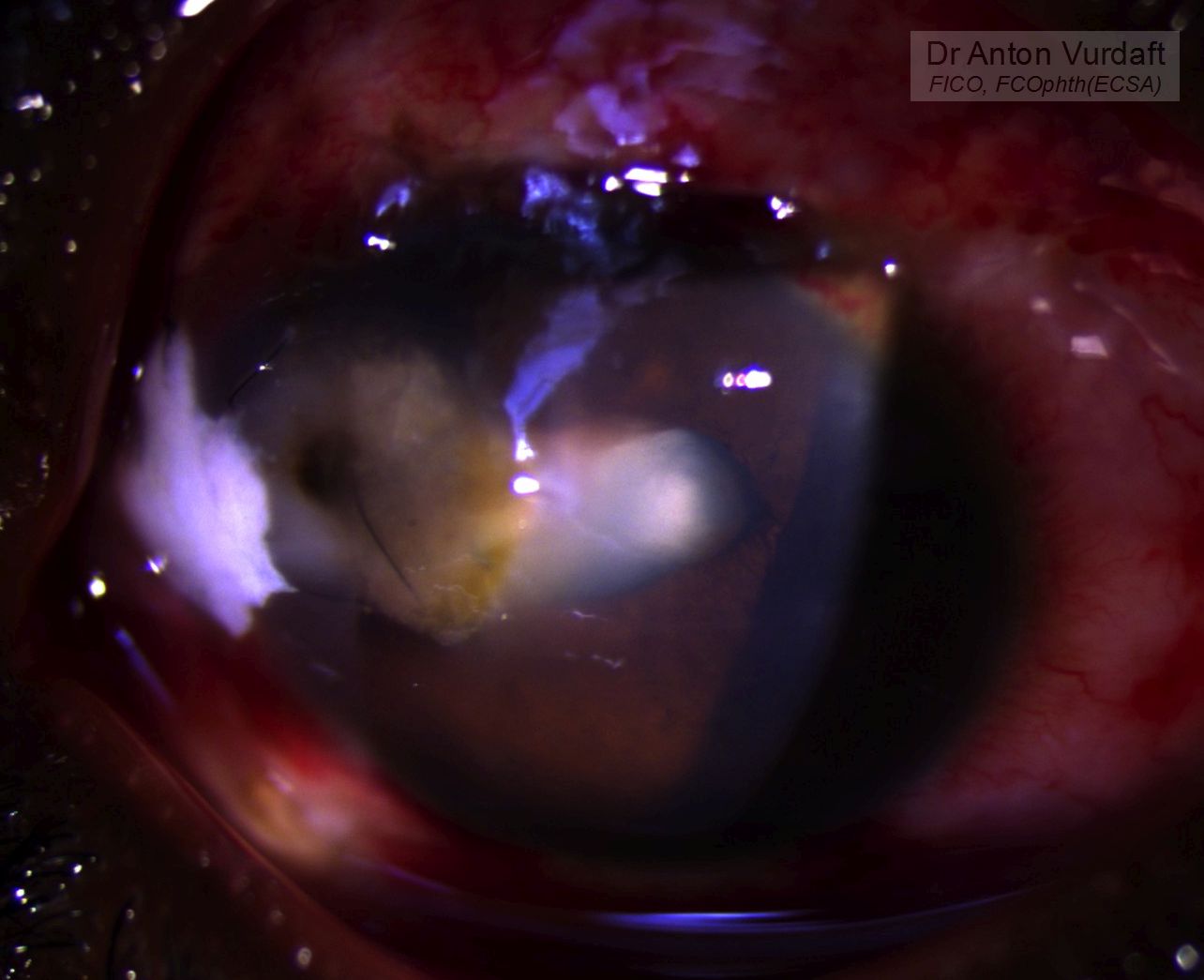
EN: A case of June 2016. A 10yo boy injured himself with a fish-hook during fishing. With these hooks people catch the tasty “mbufu” fish und occasionally even a tiger-fish in Zambesi river. The hook entered through sclera near limbus and left the eye through central cornea.
Treatment was both surgical (in 3 stages) and medical.
- Surgical extraction of the fish-hook with a help of pliers (that is what reported by the majority of papers on fish-hook eye trauma). The corneal and scleral wounds were closed with 10-0 nylon. Intravitreal antibiotic was necessary due to the extemely high endophthalmitis rate in such type of traumas. Intravitreal ceftriaxone was given due to lack of vancomycin. Lens wash-out was not performed due to poor view (central corneal wound and incipient infiltrate).
- Due to subsequent corneal infiltrate melting additional sutures were applied centrally in the cornea. Due to the limbus infiltrate melting scleral autograft closure was implemented at the limbus. Patient received systemic antibiotic and NSAID and topical antibiotic/cycloplegic treatment. Severe anterior uveitis with fibrin was resolved in a course of two weeks.
- Upon relative clearance of corneal infiltrate, lens wash-out was performed and IOL implanted.
The patient was discharged with a Vision of around 6/36, which made both of us and also his father very happy. The chance of eye loss was huge.
![]() RU: Случай от июня 2016 г. 10-летний мальчик подцепил свой собственный глаз во время рыбалки рыболовным крючком. Крючок перфорировал склеру и вышел через роговицу. Курс лечения включал три этапа хирургического лечения, включая 1) удаление крючка (перекусыванием кусачками), ушивание раны и интравитреальное введение цефтриаксона, и 2) последующее ушивание вторичной перфорации расплавившегося роговичного инфильтрата и закрытие расплавившегося инфильтрата у лимба с помощью склерального аутотрансплантата. В финале по мере относительного очищения центра роговицы от инфильтрата было произведено 3) вымывание хрусталика и имплантация ИОЛ. Лечение на всём протяжении включало системную антибиотикотерапию и НПВС-терапию, а также местную антибиотико- и циклоплегикотерапию. Пациент выписан со зрением 6/36, что для этой ситуации было высшим благом: риск потерять всё был крайне велик. Шансы на эндофтальмит у такой травмы самые высокие.
RU: Случай от июня 2016 г. 10-летний мальчик подцепил свой собственный глаз во время рыбалки рыболовным крючком. Крючок перфорировал склеру и вышел через роговицу. Курс лечения включал три этапа хирургического лечения, включая 1) удаление крючка (перекусыванием кусачками), ушивание раны и интравитреальное введение цефтриаксона, и 2) последующее ушивание вторичной перфорации расплавившегося роговичного инфильтрата и закрытие расплавившегося инфильтрата у лимба с помощью склерального аутотрансплантата. В финале по мере относительного очищения центра роговицы от инфильтрата было произведено 3) вымывание хрусталика и имплантация ИОЛ. Лечение на всём протяжении включало системную антибиотикотерапию и НПВС-терапию, а также местную антибиотико- и циклоплегикотерапию. Пациент выписан со зрением 6/36, что для этой ситуации было высшим благом: риск потерять всё был крайне велик. Шансы на эндофтальмит у такой травмы самые высокие.